THE IMPORTANCE OF PATIENT POSITIONING
Patient positioning is vital to a safe and effective surgical procedure. Proper patient positioning depends on the type and length of procedure, anesthesia access to the patient, devices required and other factors. Safely positioning the patient is a team effort. All members of the surgical team play a significant role in the process and share responsibility for establishing and maintaining the correct patient positions.
The goals of proper patient positioning include:
- Maintain the patient’s airway and circulation throughout the procedure
- Prevent nerve damage
- Allow surgeon accessibility to the surgical site as well as for anesthetic administration
- Provide comfort and safety to the patient
- Prevent soft tissue or musculoskeletal and other patient injury
PATIENT POSITIONING GUIDELINES
Following standard patient positioning guidelines and practices helps to ensure patient safety and physical well-being before, during and after a procedure. A sufficient number of personnel should always be available during a patient procedure to position the patient safely and effectively. General positioning practices include having an adequate number of personnel, devices, and equipment available during a procedure to ensure patient and staff safety. The patient should be maintained in a neutral alignment, without extreme lateral rotation or hyperextension.
Ensure that pressure is not concentrated on one point in order to avoid pressure injuries. Pressure ulcers, localized injuries to skin or underlying tissue, can occur because of pressure or pressure in combination with shear and/or friction. A sedated or anesthetized patient is not always able to communicate physical feeling such as numbness, tingling, tissue temperature, and other issues.
PATIENT POSITIONING RISK FACTORS
Various factors play a role in risk during a patient procedure as a result of positioning. Intrinsic and extrinsic factors can interact to contribute to the risk of developing pressure sores. Extrinsic factors may include pressure intensity and duration and overall effects of anesthesia. Intrinsic factors can include the overall health of the patient, and preexisting conditions such as respiratory or circulatory disorders, diabetes mellitus, anemia, malnutrition, advanced age, and body size.
Additionally, the musculoskeletal system of the patient may be subjected to stress during patient positioning. When anesthetics and muscle relaxants depress pain, pressure receptors and muscle tone, the normal defense mechanisms cannot guard against joint damage or muscle stretch and strain. One of the main goals of proper patient positioning is to keep the patient’s body as naturally aligned as possible while providing the surgical staff access to the surgical site, and quick, jerky movements should be avoided.
COMMON PATIENT POSITIONS
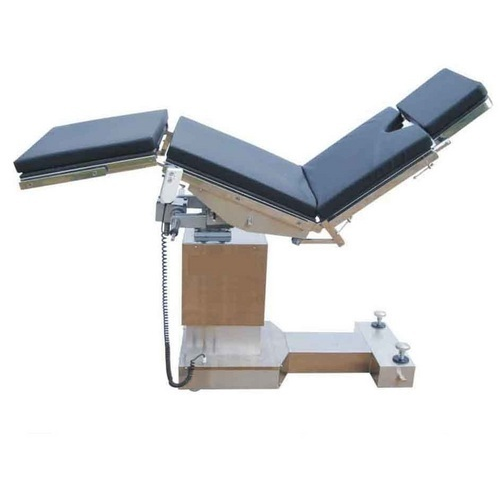
Fowler’s Position
Fowler’s position, also known as sitting position, is typically used for neurosurgery and shoulder surgeries. The beach chair position is often used for nasal surgeries, abdominoplasty, and breast reduction surgeries. When positioning a patient in Fowler’s position, the surgical staff should minimize the degree of the patient’s head elevation as much as possible and always maintain the head in a neutral position.
The patient’s arms should be flexed and secured across the body, the buttocks should be padded, and the knees flexed 30 degrees. In Fowler’s position, the patient is at an increased risk for air embolism, skin injury from shearing and sliding, and DVT forming in the patient’s lower extremities. In this position, a patient has an increased pressure risk in their scapulae, sacrum, coccyx, ischium, back of knees, and heels.
High Fowler’s Position
In High Fowler’s position, the patient is usually seated (Fowler’s position) at the head end of the operating table. The upper half of the patient’s body is between 60 degrees and 90 degrees in relation to the lower half of their body. The legs of the patient may be straight or bent.
Supine Position
Supine position, also known as Dorsal Decubitus, is the most frequently used position for procedures. In this position, the patient is face-up. The patient’s arms should be tucked at the patient’s sides with a bedsheet, secured with arm guards to sleds. The arms may be flexed and secured across the body or extended and secured on padded armboards.4
Supine position is commonly used for the following procedures: intracranial, cardiac, abdominal, endovascular, laparoscopic, lower extremity procedures, and ENT, neck and face. In Supine position, the patient may risk pressure ulcers and nerve damage. This position causes extra pressure on the skin and bony prominences over the occiput, scapulae, elbows, sacrum, coccyx and heels.
Jackknife Position
Jackknife position, also known as Kraske, is similar to Knee-Chest or Kneeling positions and is often used for colorectal surgeries. This position places extreme pressure on the knees. While positioning, surgical staff should place extra padding for the knee area.
Kidney Position
The kidney position resembles lateral position, except the patient’s abdomen is placed over a lift in the operating table that bends the body to allow access to the retroperitoneal space. A kidney rest is placed under the patient at the location of the lift.
Prone Position
In Prone position, the patient is face-down with their head in a neutral position without excessive flexion, extension or rotation. A face positioner is used when the patient’s head is in midline. Prone position is often used for spine and neck surgeries, neurosurgery, colorectal surgeries, vascular surgeries, and tendon repairs. Foam or gel positioners may also be used for spinal procedures.
When a patient is in Prone, pressure should be kept off of the eyes, cheeks, ears, and breast. At a minimum, four members of the surgical staff should be available when turning a patient prone. Risks associated with Prone position include increased abdominal pressures, bleeding, compartment syndrome, nerve injuries, cardiovascular compromise, ocular injuries, and venous air embolism.
Lithotomy Position
In Lithotomy position, the patient can be placed in either a boot-style leg holder or stirrup-style position. Modifications to this position include low, standard, high, exaggerated or hemi. This position is typically used for gynecology, colorectal, urology, perineal, or pelvis procedures.
The risks posed to a patient in a Lithotomy position for a procedure include fractures, nerve injuries, hip dislocation, muscle injuries, pressure injuries, and diminished lung capacity. While positioning a patient in this position, surgical staff should avoid hyperabduction of the patient’s hips and leaning against their inner thighs. Stirrups used on a patient in this position should disperse support and pressure over wide areas.
Sim’s Position
The Sims’ position is a variation of the left lateral position. The patient is usually awake and helps with the positioning. The patient will roll to his or her left side. Body restraints are used to safely secure the patient to the operating table. Keeping the left leg straight, the patient will slide the left hip back and bend the right leg. This position allows access to the anus.
Lateral Position
A patient may be positioned in Lateral position during back, colorectal, kidney, and hip surgeries. It’s also commonly used during thoracic and ENT surgeries, and neurosurgery. Some variations on this position include Lateral Kidney, Lateral Chest and Lateral Jackknife positions. In Lateral position, the patient may be placed on either their left or right side depending on the side of the surgical site.
A pillow or head positionershould be placed under the patient’s head with the depended ear assessed after positioning. The patient’s physiologic spinal and neck alignment should be maintained during the procedure, and a safety restraint should be secured across the patient’s hips.
Risks to a patient in Lateral position include pressure to points on the dependent side of the body such as ears, shoulders, ribs, hips, knees and ankles, as well as brachial plexus injury, venous pooling, diminished lung capacity and DVT. A pressure-reducing OR mattress or tabletop pad should be used as needed.
Trendelenburg Position
Trendelenburg position is typically used for lower abdominal, colorectal, gynecology, and genitourinary surgeries, cardioversion, and central venous catheter placement. In this position, the patient’s arms should be tucked at their sides, and the patient must be secured to avoid sliding on the surgical table.
The Trendelenburg position should be avoided for extremely obese patients. Risks to a patient while in this position include diminished lung capacity, diminished tidal volume and pulmonary compliance, venous pooling toward the patient’s head, and sliding and shearing.
Reverse Trendelenburg Position
Reverse Trendelenburg position is typically used for laparoscopic, gallbladder, stomach, prostrate, gynecology, bariatric and head and neck surgeries. Risks to a patient in this position include deep vein thrombosis, sliding and shearing, perineal nerve, and tibial nerve. Padded foot boards should be used to prevent the patient from sliding on the surgical table and reduce the potential for injury to the peroneal and tibial nerves from foot or ankle flexion.
PATIENT POSITIONING BY SURGICAL PROCEDURE
Positioning for Cardiovascular Procedures
The most common position used for cardiovascular procedures is the supine position. This position allows the best possible surgical access to the chest cavity. For coronary artery bypass grafting (CABG), the anterior thorax is exposed with the patient in a supine position. A roll is placed in the interscapular region to improve access to the sternum by extending the neck and elevating the sternal notch.
Positioning for Femoral-Popliteal Procedures
The supine position is used for Femoropopliteal (Fem/Pop) bypass surgery. Fem-pop is used to bypass narrowed or blocked arteries above or below the knee. The bypass restores blood flow to the leg. Typically, surgical table accessories such as the Fem/Pop Board will attach to the surgical table to increase lower body, intraoperative, fluoroscopic imaging coverage during the procedure.
Positioning for Cystoscopy/Urology/GYN Procedures
Variations of the lithotomy position are most commonly used in cystoscopy, urology or gynecology procedures. Surgical table accessories such as stirrups, split-leg positioners and well leg-holders are commonly used to support patient legs during procedures.
Positioning for Ophthalmic/ENT Procedures
The supine position with an additional headrest accessory, is most used for ophthalmic/ENT procedures. When the procedure is performed using a STERIS Surgical Table, a specialized adaptor accommodates standard Neuro and Eye-ENT-Neuro accessory attachments with cylindrical post attachments that are midline to the table.
Positioning for Bariatric/Split Leg Procedures
The lithotomy position in reverse Trendelenburg is most commonly used for bariatric/split leg procedures. Split Leg Positioners provide mid-line access to the patient with independent controls for full abduction/adduction as well as high and low lithotomy positioning.
Positioning for Kidney & Thoracic Procedures
A variation of lateral position with kidney elevation (flexion) is most commonly used for kidney and thoracic procedures. Lateral positioners, arm boards, headrests and restraint straps are used to safely position the patient for this procedure.
Positioning for Orthopedic Procedures
A variety of positions may be used for orthopedic procedures depending on the specific type of procedure. Common positions include supine with additional attachments for traction of lower extremities. Such procedures include hip arthroscopies and anterior hip replacements. Other common orthopedic procedures utilize Fowler’s position (beach chair) for shoulder arthroscopy procedures.
Positioning for Shoulder Chair Procedures
Fowler’s position is commonly used for shoulder arthroscopy procedures. Surgical tables may be articulated to place patients in a seated position or shoulder chair (beach chair) accessories may be used as an alternative. The patient is placed supine on the operating table and general endotracheal anesthesia is induced. The endotracheal tube should be taped to the contralateral side of the mouth to assure easy airway access during the procedure if needed.
After induction, protective foam face masks and/or head restraints are used for ocular protection during the procedure. The patient is moved into the upright beach chair position in conjunction with the anesthesia staff to ensure that the patient does not become hypotensive during this positioning maneuver.
References
1 Phillips, N. F. (2004). Berry & Kohn’s operating room technique (10th ed.). St. Louis, MO: Mosby; St-Arnaud, D., & Paquin, M. (2008). Safe Positioning for Neurosurgical Patients. AORN Journal, 87(6), 1156-1172. doi:10.1016/j.aorn.2008.03.004
2 Guideline for positioning the patient. (2017). AORN Journal, 105 (4), P8-P10. doi:10.1016/s0001-2092(17)30237-5
3 Rothrock, J. C. (2011). Alexander’s care of the patient in surgery (14th ed.). St. Louis, MO: Mosby.
4 Patient positioning during anesthesia: Supine position. (2016, December 20). Retrieved from http://www.clinicalpainadvisor.com/anesthesiology/patient-positioning-during-anesthesia-supine-position/article/582929