Mechanical ventilation is a type of therapy that helps you breathe or breathes for you when you can’t breathe on your own. You might be on a ventilator during surgery or if your lungs aren’t working properly. Mechanical ventilation keeps your airways open, delivers oxygen and removes carbon dioxide.
Overview
What is mechanical ventilation?
Mechanical ventilation is a form of life support that helps you breathe (ventilate) when you can’t breathe on your own. This can be during surgery or when you’re very sick.
While mechanical ventilation doesn’t directly treat illnesses, it can stabilize you while other treatments and medications help your body recover.
What is a ventilator?
A ventilator is a machine that helps you breathe. Just like crutches support your weight, the ventilator partially or completely supports your lung functions. A ventilator:
- Provides oxygen to your lungs.
- Helps remove carbon dioxide (CO2) from your lungs.
- Provides pressure to keep the small air sacks in your lungs (alveoli) from collapsing.
Providers can adjust the settings on the machine to meet your specific needs.
What’s the difference between mechanical ventilation and intubation?
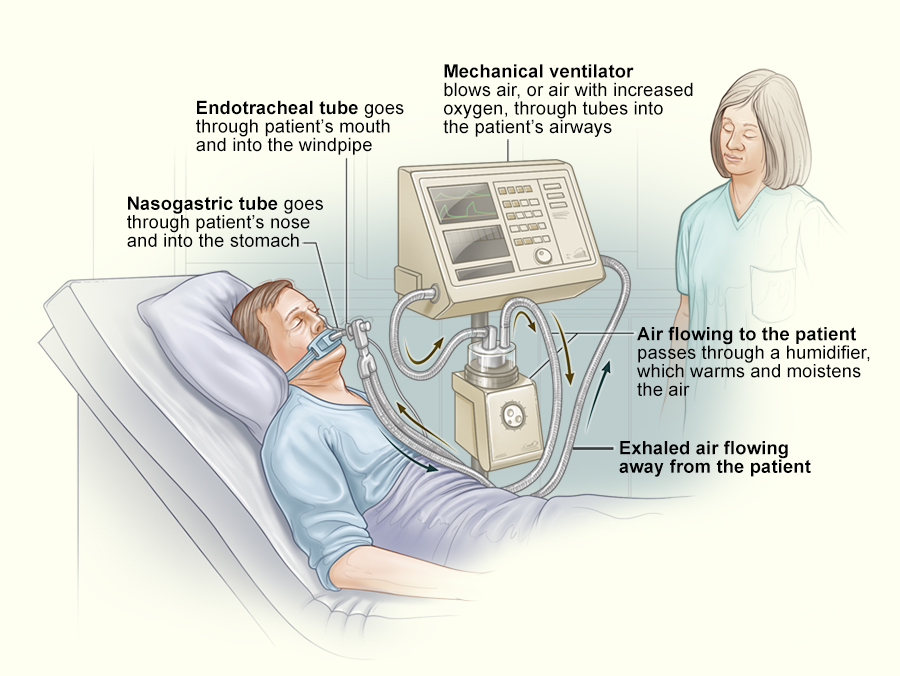
Intubation and mechanical ventilation often happen together, but they’re not the same. When a provider intubates, they put a tube down your throat into your airway (trachea). Then, a provider will connect the tube in your throat to a ventilator. Sometimes a face mask connects you to the ventilator and you don’t have to be intubated.
What are the types of mechanical ventilation?
Modern mechanical ventilators use positive pressure to push air into your lungs. Positive pressure ventilation can be invasive or noninvasive.
- Invasive mechanical ventilation: This means you have a tube in your airway connected to a ventilator. This tube can go through your mouth (intubation) or neck (tracheostomy).
- Noninvasive ventilation: This uses a face mask connected to a ventilator. Straps hold the mask to your head to hold it tight. The ventilator pushes air into your lungs. Forms of noninvasive ventilation include devices you might use at home, like CPAP or BiLevel positive airway pressure (often known under the trade name BiPAP®).

Why are mechanical ventilators used?
Providers use mechanical ventilators to support your breathing when you can’t breathe on your own. Mechanical ventilation:
- Can give you oxygen.
- Helps remove carbon dioxide so it doesn’t build up.
- Prevents parts of your lungs from collapsing from lack of pressure.
How do they actually work?
Ventilators assist or take over the breathing function for patients that are too sick to breathe on their own and to help relieve the stress on the body to promote healing. They use positive pressure to push air into the lungs. There are different types of ventilators, and each provides varying levels of support dependent on the patient’s needs.
They generally force air that is mixed with added oxygen or medication through a breathing tube into the patient and into their lungs. It does not only ensure that oxygen and air are going into the patient’s lungs but also simulates an exhale to move carbon dioxide out of the lungs.
With positive pressure ventilators, there are three settings or parameters that might be used when used on a patient. In simplified terms, the modes or settings are:
- Volume Controlled – a pre-determined amount of air is delivered to the patient.
- Pressure Controlled – air is delivered to the patient until a set pressure limit is reached.
- Dual – combines both the options of volume and pressure when used on a patient.
What are the different types of medical ventilators?
Invasive and Non-Invasive are the main two categories:
– Invasive: a tube is either placed into the patient’s airway or is inserted through a hole made in the neck. These ventilators are also called mechanical ventilators, and they take over breathing for the patient entirely. They are used when the patient is unable to breathe on their own or require extra help to breathe efficiently.
– Non-Invasive: the patient wears a mask that fits over the nose and mouth, and the air blows into their lungs. Depending on the condition of the patient, a respiratory therapist will determine what type of ventilator will be used for them.
Who needs to have mechanical ventilation?
You might need mechanical respiration:
- During surgery. General anesthesia can make it difficult to breathe well enough on your own.
- If you have certain lung conditions or infections.
- In a medical emergency that blocks your airway or impairs your breathing.
- If you have certain brain injuries or conditions. Your brain might not communicate well enough with the rest of your body, including your lungs, to allow you to breathe properly.
- If you have any conditions that cause your blood to have too much carbon dioxide (hypercapnia) or not enough oxygen (hypoxemia).
- To prevent you from accidentally getting fluids into your lungs (aspiration).
Specific conditions that might require you to have mechanical ventilation include:
- Acute respiratory distress syndrome (ARDS).
- Pneumonia.
- COVID-19 and other respiratory illnesses.
- Chronic obstructive pulmonary disease (COPD).
- Stroke.
- Traumatic brain injury.
- Coma.
- Anaphylaxis.
How long can you be kept on a ventilator?
The length of time you need mechanical ventilation depends on the reason. It could be hours, days, weeks, or — rarely — months or years. Ideally, you’ll only stay on a ventilator for as little time as possible. Your providers will test your ability to breathe unassisted daily or more often.
In general, if you need to be on a ventilator for a long time (2 weeks or so), a provider will switch you from an endotracheal tube to a tube in your neck (tracheostomy).
Procedure Details
How is someone placed on invasive mechanical ventilation?
To start invasive mechanical ventilation, a provider will:
- Give you medication to relax you (sedation) and to prevent you from moving (paralytic). You’ll most likely remain sedated, but the paralytic will wear off after you’re on the ventilator.
- Place an endotracheal (ET) tube down your throat and trachea (airway leading to your lungs).
- Attach the tube to a ventilator. The ventilator will help you breathe until your medical team feels it’s safe for you to breathe on your own again.
These are the general steps for starting mechanical ventilation. Depending on your specific situation, especially whether or not it’s an emergency, some of these steps may be a little bit different.
What happens while you’re on a ventilator?
While you’re on a ventilator, providers will perform additional procedures to treat you or prevent complications. These include:
- Monitoring.
- Suctioning.
- Providing medications.
- Providing nutrition and fluids.
- Mobilization.
- Bronchoscopy.
Monitoring
Your provider will connect you to additional machines to monitor how your body is working. This includes monitoring your:
- Blood pressure.
- Heart rate.
- Respiratory rate (how many breaths you take per minute).
- Oxygen levels.
They may also look at your lungs with chest X-rays or test your oxygen and carbon dioxide levels with blood tests.
Suctioning
Suctioning is important for keeping your airways clear. A provider will insert a catheter (a thin tube) into the breathing tube to help remove mucus (secretions). It might make you cough or gag. Loved ones may find it uncomfortable to watch.
Medications
Your provider might give you aerosolized (spray) medications through your breathing tube. These medications work best when you breathe them directly into your airways or lungs. Your provider will also give you medication into your veins through an IV.
Nutrition
You can’t eat or drink normally while you’re on a ventilator and intubated. Your provider will give you liquid nutrition, usually through a tube that goes through your nose and into your stomach. They’ll give you fluids through an IV in a vein.
Mobilization
Your providers will sit you up regularly. They may get you up and walking sometimes.
Bronchoscopy
Providers use bronchoscopy to look at the airways in your lungs. They insert a small, lighted camera through the breathing tube and into your lungs. Sometimes they’ll take samples of mucus or tissue for testing.
Who takes care of you when you’re on a ventilator?
Providers treat you in the intensive care unit (ICU) when you need mechanical ventilation. They can closely monitor you there. All providers in the ICU are specially trained to care for people who need mechanical ventilation. Providers who might care for you include:
- Respiratory therapists.
- Anesthesiologists, pulmonologists and critical care physicians.
- Nurse practitioners.
- Registered nurses.
- Nurse aides.
Are you awake while you’re on a ventilator?
While you’re on a ventilator, your provider will try to keep you as awake as possible while ensuring you’re calm and comfortable. They’ll use medications as needed to keep you relaxed. It’s not uncommon for you to be awake (conscious), but you might feel sleepy, confused or not fully aware of what’s happening.
Sometimes, depending on how sick you are, your provider may need to keep you deeply sedated (asleep) so you’re not aware and your body can recover. Your arms might be restrained to prevent you from hurting yourself by pulling on the tube.
What happens when you come off of mechanical ventilation?
Providers will perform tests to see if you can breathe on your own before taking you off the ventilator. The ET tube stays in place for these tests. When your condition has improved and you can breathe on your own, your provider will remove the ET tube to take you off of mechanical ventilation.
You might have a sore throat or mouth, or your voice may be hoarse after your provider removes the ET tube.
After removing the tube (called extubation) your provider may place you on other devices to help you breathe. These include noninvasive ventilation (with a mask) or oxygen masks. Sometimes a provider may have to intubate you again and put you back on mechanical ventilation.
Risks / Benefits
What are the advantages of mechanical ventilation?
Benefits of mechanical ventilation include:
- You don’t have to work hard to breathe. Your body can focus on healing from infections or other conditions.
- It provides all the oxygen you need and removes carbon dioxide.
- It provides pressure to keep the small sacs of your lungs from collapsing.
- It keeps your airways open.
What are the risks of mechanical ventilation?
Providers take steps to avoid complications of mechanical ventilation. However, there can still be some risks, including:
- Bacterial infections. The tube in your airways can bring bacteria into your lungs, causing infections like ventilator-associated pneumonia (VAP). This is treated with antibiotics.
- Lung damage. The pressure from the ventilator can damage your lungs.
- Collapsed lung. If part of your lung is weak, it might develop a hole, causing your lung to collapse (pneumothorax).
- Heart and blood flow changes. Being on a ventilator can affect how your heart works. If your heart doesn’t work as well, it can decrease your blood pressure or raise your heart rate. These changes can also mean less oxygen gets to your blood (decreased perfusion), even though plenty is getting into your lungs.
- Sometimes, people aren’t able to come off a ventilator. If you need to be on a ventilator for a long time, a provider will remove the tube from your mouth. They’ll insert a tube through a small cut (incision) in your neck.
- Prolonging the dying process. If someone is unlikely to recover from their condition, putting them on mechanical ventilation may prevent the dying process. This can cause unnecessary suffering. Your provider will guide you in making decisions about mechanical ventilation in this case.
Recovery and Outlook
How long does it take to recover from mechanical ventilation?
How long it takes to recover from mechanical ventilation depends on why you needed it and how long you were on it. Your provider can tell you what to expect and how to take care of yourself while you recover.
Mechanical ventilation can save your life in an emergency or if you get very sick and can’t breathe on your own. It’s not meant to treat conditions, but it can give your body the time it needs to get better. In cases of very serious or worsening illness, some people may not be able to breathe on their own again.
Regardless of your health, make sure your provider and your family know your wishes for your medical care. Having discussions about your goals and setting up advanced directives and healthcare power of attorney is an important step. This can help your loved ones if they need to make decisions on your behalf.
References
