Key principles in the performance of ACLS
| Excellent CPR is crucial. |
| Anything short of excellent CPR does not achieve adequate cerebral and coronary perfusion. Excellent chest compressions must be performed throughout the resuscitation without interruption, using proper timing (100 to 120 compressions per minute) and force (5 to 6 cm [2 to 2.5 inches] depth), and allowing for complete chest recoil.Excellent chest compressions take priority over ventilation.If a second rescuer is present, ventilations must be performed using proper timing (6 to 8 breaths per minute in the intubated patient; ratio of 30 compressions to 2 ventilations if not intubated) and force (deliver each breath over one second, and only until chest begins to rise). Avoid hyperventilation.Do not stop compressions until the defibrillator is fully charged. |
| Defibrillate VF and pulseless VT as rapidly as possible. |
| Rapidly identify and treat causes of non-shockable arrest (PEA, asystole). |
| Important causes include the 5 H’s and 5 T’s: Hypoxia, Hypovolemia, Hydrogen ions (acidosis), Hyper/Hypo-kalemia, Hypothermia; Tension pneumothorax, Tamponade-cardiac, Toxins, Thrombosis-coronary (MI), Thrombosis-pulmonary (PE).If immediately reversible causes (eg, tension pneumothorax, cardiac tamponade) are not corrected rapidly, the patient has little chance of survival. |
Knowing the H’s and T’s of ACLS will help prepare you for any ACLS scenario. The H’s and T’s of ACLS is a mnemonic used to help recall the major contributing factors to pulseless arrest including PEA, Asystole, Ventricular Fibrillation, and Ventricular Tachycardia. These H’s and T’s will most commonly be associated with PEA, but they will help direct your search for underlying causes to any of arrhythmias associated with ACLS. Each is discussed more thoroughly below.
Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hyper-/hypokalemia, Hypoglycemia, Hypothermia.
Toxins, Tamponade(cardiac),Tension pneumothorax, Thrombosis (coronary and pulmonary), and Trauma.
The H’s include:
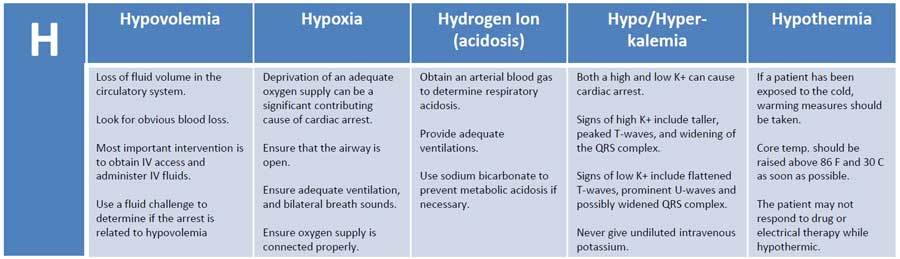
Hypovolemia
Hypovolemia or the loss of fluid volume in the circulatory system can be a major contributing cause of cardiac arrest. Looking for obvious blood loss in the patient with pulseless arrest is the first step in determining if the arrest is related to hypovolemia. After CPR, the most important intervention is obtaining intravenous access/IO access. A fluid challenge or fluid bolus may also help determine if the arrest is related to hypovolemia.
Hypoxia
Hypoxia or deprivation of adequate oxygen supply can be a significant contributing cause of cardiac arrest. You must ensure that the patient’s airway is open and that the patient has chest rise and fall and bilateral breath sounds with ventilation. Also, ensure that your oxygen source is connected properly.
Hydrogen ion (acidosis)
To determine if the patient is in respiratory acidosis, an arterial blood gas evaluation must be performed. Prevent respiratory acidosis by providing adequate ventilation. Prevent metabolic acidosis by giving the patient sodium bicarbonate.
Hyper-/hypokalemia
Both a high potassium level and a low potassium level can contribute to cardiac arrest. The major sign of hyperkalemia or high serum potassium is taller and peaked T-waves. Also, a widening of the QRS-wave may be seen. This can be treated in a number of ways which include sodium bicarbonate (IV), glucose+insulin, calcium chloride (IV), Kayexalate, dialysis, and possibly albuterol. All of these will help reduce serum potassium levels. Read more about hyperkalemia with cardiac arrest here.
The major signs of hypokalemia or low serum potassium are flattened T-waves, prominent U-waves, and possibly a widened QRS complex. Treatment of hypokalemia involves rapid but controlled infusion of potassium. Giving IV potassium has risks. Always follow the appropriate infusion standards. Never give undiluted intravenous potassium.
Hypoglycemia
Hypoglycemia or low serum blood glucose can have many negative effects on the body, and it can be associated with cardiac arrest. Treat hypoglycemia with IV dextrose to reverse a low blood glucose. Hypoglycemia was removed from the H’s but is still to be considered important during the assessment of any person in cardiac arrest.
Hypothermia
If a patient has been exposed to the cold, warming measures should be taken. The hypothermic patient may be unresponsive to drug therapy and electrical therapy (defibrillation or pacing). Core temperature should be raised above 86 F (30 C) as soon as possible.
The T’s include:
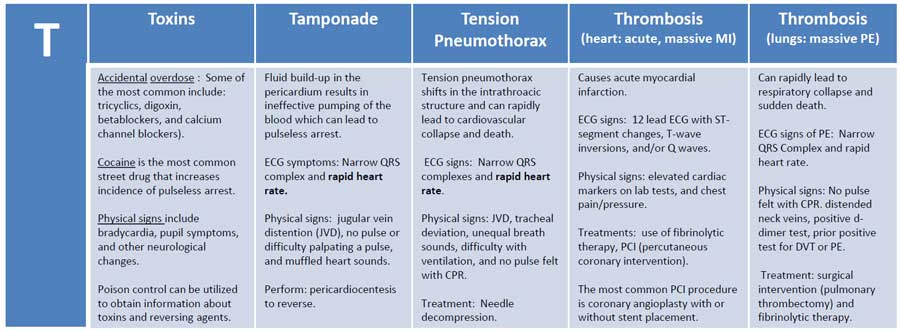
Toxins
Accidental overdose of a number of different kinds of medications can cause pulseless arrest. Some of the most common include tricyclics, digoxin, beta-blockers, and calcium channel blockers. Street drugs and other chemicals can precipitate pulseless arrest. Cocaine is the most common street drug that increases the incidence of pulseless arrest. ECG signs of toxicity include prolongation of the QT interval. Physical signs include bradycardia, pupil symptoms, and other neurological changes. Support of circulation while an antidote or reversing agent is obtained is of primary importance. Poison control can be utilized to obtain information about toxins and reversing agents.
Tamponade
Cardiac tamponade is an emergency condition in which fluid accumulates in the pericardium (sac in which the heart is enclosed). The buildup of fluid results in the ineffective pumping of the blood which can lead to cardiac arrest. ECG symptoms include narrow QRS complex and rapid heart rate. Physical signs include jugular vein distention (JVD), no pulse or difficulty palpating a pulse, and muffled heart sounds due to the fluid inside the pericardium. The recommended treatment for cardiac tamponade is pericardiocentesis.
Tension Pneumothorax
Tension pneumothorax occurs when air is allowed to enter the pleural space and is prevented from escaping naturally. This leads to a build-up of tension that causes shifts in the intrathoracic structure that can rapidly lead to cardiovascular collapse and death. ECG signs include narrow QRS complexes and rapid heart rate. Physical signs include JVD, tracheal deviation, unequal breath sounds, difficulty with ventilation, and no pulse felt with CPR. Treatment of tension pneumothorax is needle decompression.
Thrombosis (heart: acute, massive MI)
Coronary thrombosis is an occlusion or blockage of blood flow within a coronary artery caused by blood that has clotted within the vessel. The clotted blood causes an acute myocardial infarction which destroys heart muscle and can lead to sudden death depending on the location of the blockage.
ECG signs during PEA indicating coronary thrombosis include ST-segment changes, T-wave inversions, and/or Q waves. Physical signs include elevated cardiac markers on lab tests.
For patients with cardiac arrest and without known pulmonary embolism (PE), routine fibrinolytic treatment given during CPR has shown no benefit and is not recommended.
Treatments for coronary thrombosis before cardiac arrest include the use of fibrinolytic therapy, or PCI (percutaneous coronary intervention). The most common PCI procedure is coronary angioplasty with or without stent placement.
Thrombosis (lungs: massive pulmonary embolism)
Pulmonary thrombus or pulmonary embolism (PE) is a blockage of the main artery of the lung which can rapidly lead to respiratory collapse and sudden death. ECG signs of PE include narrow QRS Complex and rapid heart rate. Physical signs include no pulse felt with CPR. distended neck veins, positive d-dimer test, prior positive test for DVT or PE. Treatment includes surgical intervention (pulmonary thrombectomy) and fibrinolytic therapy.
Trauma
The final differential diagnosis of the H’s and T’s is trauma. Trauma can be a cause of pulseless arrest, and a proper evaluation of the patient’s physical condition and history should reveal any traumatic injuries. Treat each traumatic injury as needed to correct any reversible cause or contributing factor to the pulseless arrest. Trauma was removed from the T’s but is still to be considered important during the assessment of any person in cardiac arrest.
Hs and Ts
As you are moving through your algorithms during ACLS and PALS, it is important to also consider reversible causes for the emergent condition. Pulseless electrical activity (PEA), asystole, ventricular fibrillation (VFib or VF), and ventricular tachycardia (VTach or VT) may have a reversible cause in your patient (though most often PEA). The reversible causes of PEA can be remembered with a mnemonic of sorts, the H’s and T’s.
The H’s and T’s are 12 reversible conditions, 7 that start with H and 5 that start with T.
- Hypovolemia
- Hypoxia
- Hydrogen ion excess (acidosis)
- Hypoglycemia
- Hypokalemia
- Hyperkalemia
- Hypothermia
- Tension pneumothorax
- Tamponade – Cardiac
- Toxins
- Thrombosis (pulmonary embolus)
- Thrombosis (myocardial infarction)
While it is important to continue to deliver compressions, ventilation, and medications according to the algorithm, it is always best to treat underlying causes of PEA and related conditions as soon as possible.
| Potential Cause | How to Identify | Treatments |
| Hypovolemia | Rapid heart rate and narrow QRS on ECG; other symptoms of low volume | Infusion of normal saline or Ringer’s lactate |
| Hypoxia | Slow heart rate | Airway management and effective oxygenation |
| Hydrogen ion excess (acidosis) | Low amplitude QRS on the ECG | Hyperventilation; consider sodium bicarbonate bolus |
| Hypoglycemia* | Bedside glucose testing | IV bolus of dextrose |
| Hypokalemia | Flat T waves and appearance of a U wave on the ECG | IV Magnesium infusion |
| Hyperkalemia | Peaked T waves and wide QRS complex on the ECG | Consider calcium chloride, sodium bicarbonate, and an insulin and glucose protocol |
| Hypothermia | Typically preceded by exposure to a cold environment | Gradual rewarming |
| Tension pneumothorax | Slow heart rate and narrow QRS complexes on the ECG; difficulty breathing | Thoracostomy or needle decompression |
| Tamponade – Cardiac | Rapid heart rate and narrow QRS complexes on the ECG | Pericardiocentesis |
| Toxins | Typically will be seen as a prolonged QT interval on the ECG; may see neurological symptoms | Based on the specific toxin |
| Thrombosis (pulmonary embolus) | Rapid heart rate with narrow QRS complexes on the ECG | Surgical embolectomy or administration of fibrinolytics |
| Thrombosis (myocardial infarction) | ECG will be abnormal based on the location of the infarction | Dependent on extent and age of MI |
*Hypoglycemia is not officially one of the H’s and T’s for adults, but it still can be an important cause of PEA, especially in children. If another reversible cause has not been discovered or if the patient is known to be susceptible to hypoglycemia (e.g., brittle diabetes, past surreptitious use of insulin) then this potential cause of PEA should be considered.
