Abbreviations
- STEMI – ST Elevation Myocardial Infarction
- FMC – First Medical Contact
- DTB – Door-to-Balloon Time
- ICH – Intracranial Hemorrhage
- MACE – Major Adverse Cardiac Events (i.e. CV death, reinfarction, recurrent MI, shock, ischemic sx)
- TNK – Tenecteplase
- PCI – Percutaneous Coronary Intervention
- Primary PCI – PCI selected as initial revascularization strategy
- Secondary PCI – PCI performed after successful thrombolysis
- Rescue PCI – Urgent PCI performed after failed thrombolysis
Introduction
- A STEMI is a true cardiac emergency, you must recognize a patient with a STEMI and arrange revascularization ASAP.
- When available, percutaneous coronary intervention (PCI) is preferred to thrombolysis
- Randomized trials have consistently shown better outcomes in terms or mortality and ischemic events with PCI.
- Major complications such as intracranial hemorrhage are reduced with PCI.
- Thrombolysis is offered only when PCI cannot be arranged quickly enough.
Diagnosis
Definition
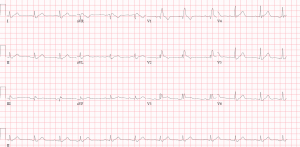
| DEFINITION OF A STEMI |
|---|
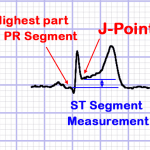
| ST-segment elevation (measured at J-point)≥ 1mm in all leads except V2-V3 (amplified leads)In V2-V3, to be significant:Men ≥ 40: ≥ 2 mmMen < 40: ≥ 2.5 mm [accounting for early repolarization in young men]Women: ≥ 1.5 [accounting for lower amplitude ECGs in women]Two contiguous leadsClinical picture compatible with myocardial ischemia (i.e. symptoms)NOTE: J-point is the junction between the termination of the QRS segment and beginning of the ST segment. |
| ESC 2017 Guidelines, AHA/ACC 2013 Guidelines |
Differential
- Not all ST elevation is a STEMI!
- ST segment on an ECG can be elevated for a number of reasons:
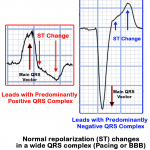
- Any wide QRS (generally > 120ms) or a large-amplitude QRS (such as LVH) produces a repolarization abnormality, which results in the shifting of the ST segment in the opposite direction of the main QRS vector, which is known as “discordant ST change”. (See Figure: “Normal ST Changes in LBBB or Pacing” Below)
- Wide QRS or large-amplitude QRS patterns that can cause discordant ST changes include: RBBB, LBBB, LVH, RVH, Pacing, Metabolic QRS widening, Pre-excitation, etc.
- Significant transmural ischemia due to supply/demand mismatch can also produce ST elevation.
- ALWAYS rule out:
- Aortic Dissection (can present as Inferior STEMI – look for 1. Tearing Pain, 2. Maximal intensity at onset, 3. involving the back.
- PE – Calculate the wells score
- Pericarditis – Pleuritic? positional? pericardial rub? effusion?
- Mechanical complication: (VSD, papillary muscle rupture) look for new murmur, or sudden flash pulmonary edema.
- ST segment on an ECG can be elevated for a number of reasons:
Notes
- Presence of reciprocal changes supports the diagnosis.
- Troponin elevation is NOT required for diagnosis because STEMI is acute, cTn may be negative if you measure early enough in the course of a STEMI
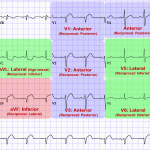
- Memorize the lead orientation!
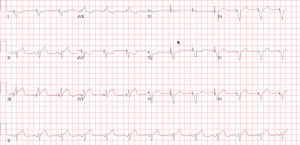
STEMI ECG
- Must measure J-point elevation compared with the PR segment (NOT TP segment)
STEMI with LBBB
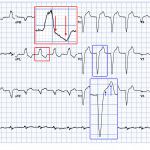
- Left Bundle Branch Blocks (LBBB) are uniquely challenging at interpreting for ischemic changes because any wide QRS (BBB, pacing, pre-excitation, etc..) produces a repolarization abnormality that moves the ST segment and T wave.
- Distinguishing repolarization abnormalities from the wide QRS from ST changes due to ischemia can be tricky.
- Principle:
- When an ECG has a wide QRS, the ST segment and T-wave always shift in the opposite direction of the main QRS vector (aka “discordant”). In a patient who is suspected of having ACS, concordance of the ST segment suggests a STEMI, while discordance can be normal.
- The only exception is V1-V3, where QRS is always negative in a LBBB. In that case we look for excessive discordance (ST elevation of > 5mm), which means ST segments are much more elevated than the LBBB can account for.
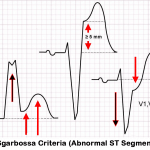
- Sgarbossa criteria (described by Elena Sgarbossa) uses the above principle to objectively assess ST changes in patients with LBBB/paced rhythm, who are suspected of having a STEMI. This criteria was well validated for STEMI.
- Modified Sgarbossa Criteria: Introduced to improve the sensitivity of Sgarbossa criteria. The only change is “Discordant ST elevation > 5mm” point is replaced with “ST Elevation > 25% of preceding S-wave amplitude”
| SGARBOSSA CRITERIA |
| Concordant ST-Elevation of 1 or more mm = 5 pointsConcordant ST-depression of 1 or more mm in V1-V3 = 3 pointsDiscordant ST-elevation of more that 5 mm = 2 pointsScore of 3 or more has a 90% specificity for myocardial infarction. Not sensitive.Modified Sgarbossa Criteria: “Discordant ST-elevation of > than 5mm” replaced with “ST elevation > 25% of the S-wave amplitude” |
| Sgarbossa et al 1996 – NEJM |
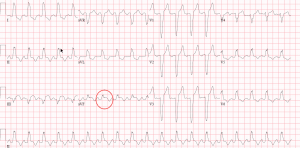
Examples: Case 1 and 2
Example: Case 3
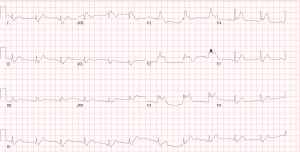
Posterior STEMI & RV Infarct
- All patients with anterior ST depressions and inferior ST elevations must get a 15-lead ECG to assess for RV infarct and posterior STEMI.
- Posterior MI – A 15-lead ECG provides additional V7-V9 leads, which allow additional assessment for a posterior STEMI.
- Posterior STEMIs are commonly missed because a 12-lead ECG demonstrates ST depressions in anterior leads, and patients are treated as an NSTEMI, and do not receive emergent revascularization.
- REMEMBER: Anterior leads are reciprocal to posterior leads, so posterior ST elevations present with anterior ST depressions, and vice versa.
- RV Infarct
- A 15-lead ECG also provides the V4r lead (R-sided V4 lead), which is located over the RV free wall.
- ST elevations in this lead suggest RV involvement, which has important clinical consequence – these patients have a damaged RV, and are very preload dependent. They often present hypotensive, requiring fluids. They also do not tolerate any preload reduction, such as nitroglycerin.
- Delivering nitroglycerin to patients with an RV infarct (ST Elevation in V4r) can result in severe hypotension. Therefore, nitroglycerin is contraindicated in patients with an RV infarct.
- Posterior MI – A 15-lead ECG provides additional V7-V9 leads, which allow additional assessment for a posterior STEMI.
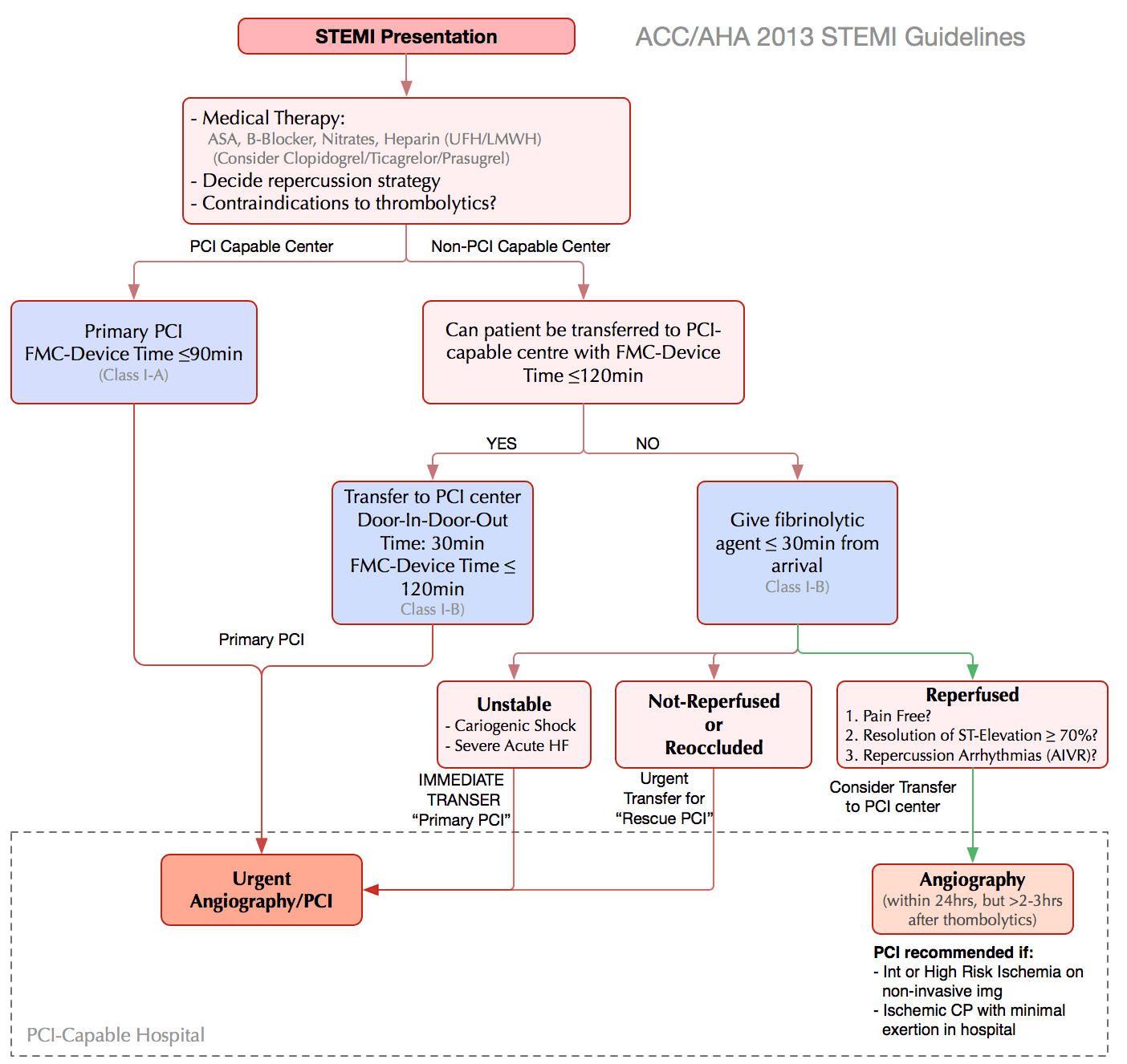
Select Urgent Reperfusion Method
- Generally Primary PCI is preferred to thrombolysis
- (higher rates of artery patency, lower recurrent ischemia, reinfarction, emergency revasc, ICH, and death).
- However, delay to PCI also has high risk of adverse outcomes – generally the cutoff used is 120min.
- NOTE: Generally thrombolysis is most effective at 1-2hrs after symptom onset, with gradually reducing efficacy to 6 hrs. After 6h, efficacy is lower (Guidelines still recommend thrombolysis if within 12hrs – see below).
| SELECTING REPERFUSION THERAPY (AHA 2013) |
| Eligible for reperfusion therapy?Symptom onset <12hrs (Class I)Symptom onset 12-24hrs if: clinical/ECG evidence of ongoing ischemia large area of myocardium at risk or hemodynamic instability (Class IIa)PCI is preferred if it can be delivered within 120 min of first medical contact (FMC)Thrombolysis is preferred if expected FMC-to-balloon time > 120 minFor major PCI/urban centers, ideal FMC-to-balloon time is 90 minutesIf thrombolysis is selected, door-to-needle time should be 30 minutes |
| AHA 2013 STEMI Guidelines |
| ABSOLUTE CONTRAINDICATIONS TO THROMBOLYSIS |
| Any history of ICHIschemic stroke within 3 months.Intracranial neoplasm or structural cerebral vascular lesion (exp. arteriovenous malformation).Suspected aortic dissection. (Occasionally dissection will present as inferior STEMI)Active internal bleeding (excluding menses)Closed head/face trauma in last 3 months.NOTE: You must know these for exam purposes |
| CCS 2019 – STEMI Guidelines |
| RELATIVE CONTRAINDICATIONS TO THROMBOLYSIS |
| Severe hypertension of sBP > 180 mmHg, or dBP > 110 mmHg.Any history of ischemic stroke.Major trauma in past 2-4 weeks.Non-compressible vascular puncture.Pregnancy.Active peptic ulcer.Use of anticoagulants. |
Management: Thrombolysis Strategy
- Rule out contraindications!
- NOTE: Time from symptom onset is important!
- Must ideally be within 12 hrs of pain onset (Class I)
- Can thrombolyze if symptom onset 12-24hrs ONLY if one of the following:
- Clinical/ECG evidence of substantial/worsening ischemia
- Electrical / Hemodynamic Instability
- The magnitude of the reduction in the risk of death in randomized trials is generally between 15-30%
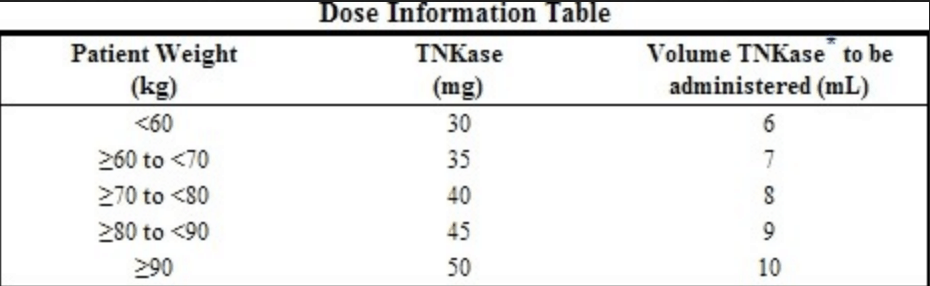
- Tenecteplase (TNK) is the thrombolytic of choice in coronary disease. (ASSENT II Trial – less bleeding than TPA)
- NOTE: The benefit of thrombolysis is strongly related to time from symptom onset. After 6 hours, studies show rapidly diminishing benefit, and risk/benefit profile becomes more balanced. After 12 hours there is little benefit to thrombolysis because the plaque begins to harden, and the thrombolytic effect is attenuated. However, these patients may still be eligible for PCI, which has a lower bleeding risk and more effective reperfusion. PCI should be strongly considered in patients who have ongoing pain or non-resolving ST elevation.
Adjunctive Therapy to Fibrinolysis
- ASA load (162 mg) (Chewed if non-enteric coated is available) -> Then 81 mg for life.
- Clopidogrel load (300 mg) then 75 mg daily. Generally don’t load patients > 75 yo
- Do not give Ticagrelor or Prasugrel when thrombolysis planned.
- Anticoagulation (Three Options).
- Heparin: 60units/kg bolus (Max 4000 units) followed by 12mg/hour infusion titrate to protocol. PTT 50-70 (LHSC). Note the Max dose is lower for thrombolysis vs PCI (Max 5000 units).
- Duration: 48hrs, or revasc or discharge
- Enoxaparin: Age <75 years use a loading dose of 30 mg IV bolus followed by 1 mg/kg subcutaneously every 12 hours (maximum of 100 mg for the first two doses only).
- Duration: 8 days or until revasc or discharge
- In patients ≥75 years no loading dose and 0.75 mg/kg subcutaneously every 12 hours (maximum of 75 mg for the first two doses only).
- Fondaparinux: giving 2.5 mg intravenously, followed by 2.5 mg subcutaneously once daily.
- Heparin: 60units/kg bolus (Max 4000 units) followed by 12mg/hour infusion titrate to protocol. PTT 50-70 (LHSC). Note the Max dose is lower for thrombolysis vs PCI (Max 5000 units).
- High Intensity/Dose Statin: Atorvastatin 80mg daily or Rosuvastatin 40mg daily.
- Beta-Blocker: Contraindicated in active heart failure or shock or hemodynamic concerns (i.e. bradycardia or hypotension).
- ACE-Inhibitors: Should be started within 24 hours
What to do after thrombolysis
- Transfer patient to a PCI-capable centre within 6 hours (TRANSFER-AMI study 2009 – improves MACE)
- Once at PCI-capable centre, effectiveness of thrombolysis should be assessed (see right-panel)
- If Reperfused:
- Monitoring + angiogram within 3-24hrs post lysis for possible secondary PCI
- If not reperfused:
- Rescue PCI
| INDICATORS OF REPERFUSION (NEED FOR RESCUE PCI) |
| Aassesed 60-90min post-thrombolysisResolution/Improvement of chest pain>50% reduction in ST elevation in lead with maximal initial ST elevationHemodynamic or electrical stability(Reperfusion arrhythmias like AIVR) |
| Criteria vary, but these are research criteria (CCS 2019 Guideline) |
Thrombolysis Pearls
- Do not wait for biomarkers (take time to rise) -> Thrombolyse on clinical presentation and EKG.
- Clopidogrel is the antiplatelet of choice when the decision is made to thrombolyse.
- If PCI can be performed within 120 minutes of first medical contact this is the preferred treatment.
- May not be sufficient benefit to thrombolyse after 12 hours especially if there is no ongoing symptoms of chest pain (completed infarct). This decision can be shared with expert consultation.
Management: Primary PCI Strategy
- Primary PCI is preferred over thrombolytic therapy for STEMI if it can be done without delay
- PCI = higher rates of infarct artery patency, less access site bleeding, less recurrent ischemia, less ICH, fewer repeat procedures, fewer post-MI compliations, earlier discharge, lower risk of death (AHA 2013 summary)
- Risks of Primary PCI: (<2%)
- See Post on PCI
| INDICATIONS FOR PRIMARY PCI IN STEMI |
| STEMI + Symptom duration < 12hrs (Class I)STEMI + Symptom duration < 12hrs + ineligible for thrombolysis (Class I)STEMI (irrespective of symptom duration) if one of: (Class I)Cardiogenic shockAcute severe heart failureSTEMI + symptom duration >12 hrs + indicators of ischemia or electrical/hemodynamic instability (Class IIa) |
| CCS 2013 STEMI Guidelines |
Adjunctive Therapy in PCI
- Target O2sat 90% (avoid excessive O2)
- ASA 162mg before primary PCI, continue 81mg daily indefinitely (Class I)
- Chewed if non-enteric coated is available
- P2Y12 inhibitor before or during primary PCI, options: (Class I)
- Ticagrelor 180mg once, then 90mg BID (PLATO trial)
- Prasugrel 60mg once, then 10mg daily (TRITON-TIMI-38 trial) – Not available in Canada
- (contraindicated in pts with prior TIA/stroke
- (less effect if age ≥ 75 or weight < 60kg)
- Clopidogrel600mg once, then 75mg daily (CURRENT-OASIS 7 trial)
- Less preferred because requires 2 activation steps (CYP 2C19 reduced-function carriers have low active drug levels, and worse outcomes)
- PPI (prominently omeprazole) can reduce active drug levels
- Duration of antiplatelet therapy:
- Continue for at least 1 year. At 1 year weigh risks of bleeding vs. risk of ischemic events (See Table to the left)
- Generally, if tolerating DAPT at 1 year, continue for up to 3 years with one of the following:
- ASA 81mg daily + Ticagrelor 60mg BID (PEGASUS-TIMI-54 Trial)
- ASA 81mg daily + Clopidogrel 75mg daily (DAPT Trial)
- ASA 81mg daily + Prasugrel 10mg daily (DAPT Trial)
- GP IIB/IIIA inhibitors
- Only given to select patients with STEMI in the cath lab
- Used for patients with large thrombus burden or inadequate DAPT loading.
- Anticoagulation
- Unfractionated Heparin (preferred – low cost, effective)
- Bivalirudin (HORIZONS-AMI Trial)
- Duration: Stop anticoagulation once patient is revascularized
- (NOTE: Enoxaparin (ATOLL Trial) failed to show benefit in patients with STEMI, and Fondaparinux has a high risk of catheter thrombosis in this setting, hence neither are recommended for STEMI patients undergoing PCI) (AHA 2013)
- High Intensity/Dose Statin: Atorvastatin 80mg daily or Rosuvastatin 40mg daily.
- Beta-Blocker: Contraindicated in active heart failure or shock or hemodynamic concerns.
- ACE-Inhibitors: Should be started within 24 hours.
Post-MI Care and Driving
- Refer to Cardio Guide summary on Post-MI Care and Driving Guidelines
References
- CCS 2019 STEMI Guidelines
- AHA/ACCF 2013 STEMI Guidelines
- ESC 2017 STEMI Guidelines
- ST Elevation MI (STEMI)
Primary Author: Dr. Pavel Antiperovitch (MD, FRCPC, Cardiology Fellow)Author/Reviewer: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)Staff Reviewer: Dr. Michael Ward (MD, FRCPC[Cardiology] – Interventional Cardiologist at the Western University)